Shoulder Check
- Janet Delorme
- Apr 19, 2023
- 6 min read
The Shoulder Joint Complex …a look back in time.

My last blog identified how ‘shoulder’ assessments are systematically overlooking the possibility of a primary scapulothoracic problem in patients who do not appear to have an obvious winging scapula. This leads us to another question… how can the scapulothoracic joint be assessed?
To answer this question, we need to look back to the beginning. Compared with other areas of medical specialty, the assessment and treatment of the shoulder joint complex has a relatively short history. It was not until Wilhelm Roentgen, a physics professor from Bavaria, accidentally discovered X-rays in 1895, that physicians were able to observe bones through layers of tissue. It was not long before physicians worldwide were using X-rays to diagnose fractures and observe bullets, kidney stones and swallowed objects.

While there are several orthopaedic surgeons who are recognized for their pioneering work during the early years of the twentieth century, it was Amory Codman (1869-1940), a pioneer in six different fields of medicine: anaesthesiology, radiology, duodenal ulcer surgery, orthopaedic oncology, shoulder surgery and the study of medical outcomes, who first observed a pattern of movement at the four-joint shoulder complex. He coined the descriptive term, still used today: scapulohumeral rhythm. A pioneer in shoulder surgery, Codman published the first book ever written (in English) solely on the shoulder. His 1934 publication is considered “decades ahead of its time” and “still pertinent today for any practicing shoulder surgeon.”
Even today, Codman’s ‘pendular’ shoulder exercises remain a mainstay for physiotherapists who wish to teach their ‘frozen shoulder’ patients how to introduce easily isolated movement for the painful and stiff glenohumeral joint.
It was in 1944 when three of the most accomplished orthopedic specialists at that time: Verne T. Inman, J.B. dec M Saunders and L.C. Abbott. (Inman et al.) combined their expertise in orthopedic surgery, anatomy, functional anatomy, biomechanics, and prosthetics, to write what is considered the ‘Classic’ Observations of the Function of the Shoulder Joint.
Inman et al. stated that the term “shoulder joint” was misleading because the motion at the “shoulder” includes motion at four different joints: the sternoclavicular (SC) the acromioclavicular (AC) the scapulothoracic (ST) and the glenohumeral (GH).
They determined that much of what was known about the shoulder at that time was ‘contradictory and incomplete’ because observations were based on an inert cadaver, not a living, moving person. “…there is only one touchstone to which we can appeal, and that is the living body” (The Classic).
To study the living, moving body, Inman et al. used the tools available to them at that time. They inserted pins into the bones of living subjects and used x-rays (roentgenography) to gain insight into how the shoulder bones moved during active elevation of the arm.
They determine that…
1. Movement at each of the four shoulder joints is simultaneous and not successive.
2. The highly irregular phase of scapular motion, noted as the arm starts to elevate away from the body was identified as the “setting phase”(this familiar term is still in use today). The setting phase occurs during the first 30 degrees of abduction or 60 degrees of forward flexion when the shoulder muscles are ‘adjusting’ to accommodate the precise relationship between the scapula and the humerus.
3. After the setting phase, the arm elevates to 170 degrees at a humerus-to-scapula ratio of 2:1. For every 10 degrees of humeral elevation, there will be 5 degrees of upward scapular rotation on the thorax. The motions of either one of these joints can, under certain circumstances, occur independently.
4. Combined movement at the SC and AC joints provides total movement permitted at the ST joint.
5. Elevation of the arm is accompanied by elevation and rotation at the clavicle, which rotates on its long axis to allow its curvature to act as a crankshaft.
Using the measurements obtained from their X-rays, Inman et al. set up equations to calculate theoretical force requirements for maintaining the dependent arm and for elevating the arm. They determined that three essential forces, created by muscle force couples were the essential principle for both the elevation of the arm at the GH joint as well as the upward rotation of the scapula.
The electrical action potentials of active muscles (electromyography or EMG) were then utilized to correlate their X-ray and theoretical force requirement findings. The muscles were divided into three groups: the muscles that elevated the humerus, muscles that depressed the humerus and muscles that rotated the scapula.
If we compare the findings from Inman et al. (1944) to our present-day knowledge on this subject, there are many differences because today, our methods and tools are much more sophisticated. However, there is much that remains noteworthy. This 1944 research project was extensive, and while the entire document may be available today, its length and complexity would be of interest to only the most serious students of kinesiology. I found that the abbreviated version offered more than enough detail…
Of special interest for me, was the Inman et al. description of the two largest scapulothoracic muscles – the ones that primarily control the position of the scapula on the chest wall - the trapezius and the serratus anterior. Both were described as having three separate parts: upper, intermediate, and lower. They determined that “different portions of the same muscle differ in their degree of activity, depending on the precise motion carried out.”
The upper components of these two muscles, combined with levator scapulae were described as having three functions:
1. Passive support for the shoulder (antigravity)
2. Active elevation of the shoulder
3. Providing the upper component of the force couple necessary for scapular rotation.
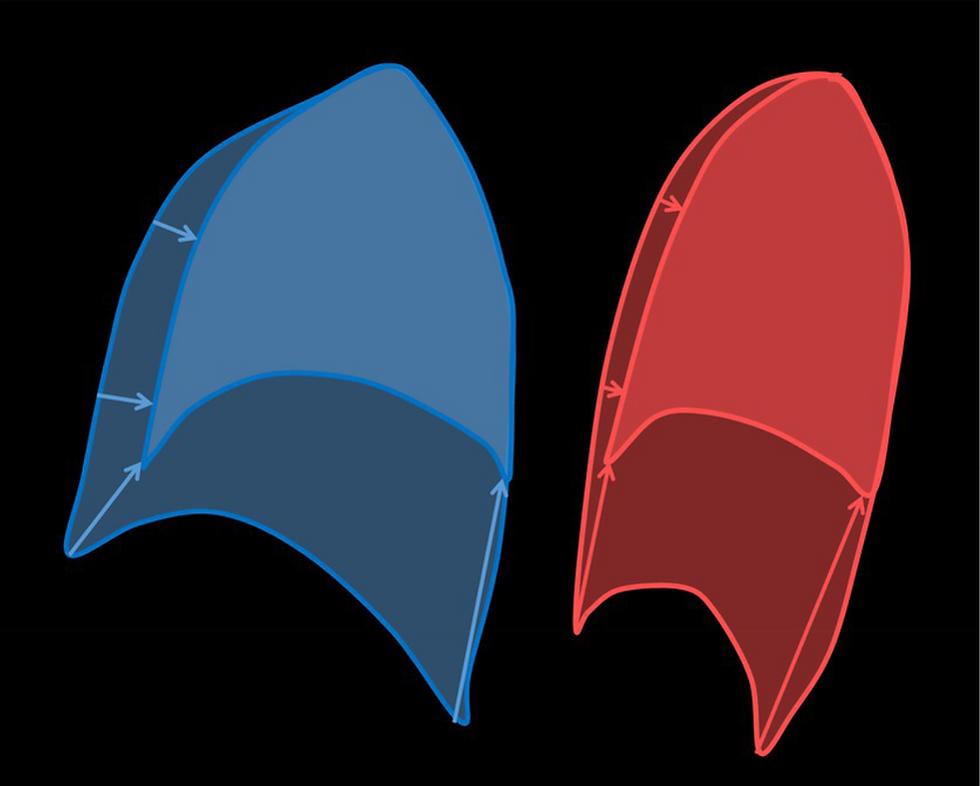
The middle and lower fibres of serratus anterior and trapezius were described as “mirror images” of each other, with the trapezius, working harder to hold the scapula in place on the chest wall when the arm is held in abduction (out to the side). To lift the arm up into flexion, the trapezius relaxes, allowing the serratus anterior to do most of the work as the scapula moves around the chest wall, and the arm is lifted, in front of the body.
After a lengthy career as a lifelong learner/practicing physiotherapist, I considered myself to have excellent shoulder anatomy and mechanics knowledge.
After injuring my shoulder in 2012, I learned how to live without the use of my left serratus anterior muscle. For the FIRST time in my life, I discovered that serratus anterior is, in fact, a three-part muscle, and I ‘discovered’ many recent morphological studies that confirm this.(Smith et al 2003 Webb et al. 2018, Bertelli, Ghizoni 2005

Understanding the serratus anterior’s three-part morphology and its “mirror image” behaviour with trapezius was something I came to understand on my own, once I started to recognize how these two, well-matched muscles really do work together. Rather than describing them as mirror images of each other, however, I embraced a more three-dimensional approach, and compared them with the ancient yet familiar concept of 'yin and yang'. The full description is in my book, pp 22-24 (Scapulothoracic Assessment in Three Simple Steps).
For the first time in my life, I discovered that serratus anterior has very little to do with protraction or doing a “push up” and a great deal to do with the ability to tolerate the weight of the dependent arm and the ability to heave it up overhead – especially out in front, into flexion. Serratus anterior also has a role in respiration (breathing), but that is a topic for another blog.
By closely studying what has been meticulously observed, measured and analyzed in the past, I realize that there is much to learn by looking back in time to gain some insight from those who came before us. Also, it would have been much easier to write my book if I wasn’t so busy re-writing and ‘discovering’ what had already been noted and written about seventy years earlier.
For reasons of physical necessity, most newer texts today only offer a superficial summary of information that will assist in the general knowledge that is needed for a musculoskeletal assessment. Deciding which information makes ‘the cut’ is difficult because there is such a wealth of information to choose from, and that information is always changing.
While new technologies, bigger studies and better research continue to offer a plethora of ‘new’ information, it is only with the understanding of information that came before us that we can move forward.
Observation is an essential tool when assessing the shoulder joint complex, but only if the examiner knows where to look and what to look for. Codman, Inman, Saunders and Abbott laid out some essential groundwork. It is now time to take their knowledge to the next level.



Comments