Revolutionizing Shoulder Diagnostics: Embracing Inclusivity in Chronic Condition Management
- Jan 10, 2024
- 5 min read
...there are very few true, singular diagnoses for shoulder pathology.
Epidemiological ‘shoulder’ studies to date, cannot identify or define a singular ‘shoulder’ condition or problem because many conditions masquerade under the common guise that we must identify as a ‘shoulder’ problem. Like a mixed bag of tricks, all symptoms that seem to originate in this region are packaged up into a single descriptive term – ‘the shoulder’.
While the medical community will argue that there are many, many reasons for shoulder pain – the truth is that there are very few true, singular diagnoses for shoulder pathology and most shoulder pain sufferers present with symptoms that do not fit into these singular diagnostic slots.
A review of the highlighted purple text from my last two blogs will confirm…
…it is not clear that complete recovery occurs, one study reports that 50% of patients did not recover full movement after 7 years.
Patients presenting with more than one shoulder lesion made the diagnosis more difficult to ascertain. Patients with high pain severity, chronic complaints and bilateral involvement were the most difficult to classify.
This sub-group of patients is identified as having ‘non-specific shoulder pain’, which is described as ‘shoulder pain, discomfort, fatigue, limited movement and loss of muscle power but without a pattern allowing a specific diagnosis to be made’
Non-specific shoulder pain, frequently found in general population and workplace studies, is estimated to be six times more frequent than specific shoulder conditions with clear diagnostic markers - rotator cuff for example.
These systems also failed to cater to patients who partially fulfilled the criteria or who had patterns of complaint that fell outside of the specified categories.
… lack of connection between tissue pathology and pain. Often there are multiple tissue pathologies around the shoulder.
…most outcomes do not demonstrate fully resolved symptoms or positive outcomes for all individuals.”
If an expected ‘pattern’ doesn’t fit and ‘clear diagnostic markers’ are not found....look somewhere else
While it would be convenient to assume that a shoulder problem is a problem in or around the glenohumeral joint, evidence to date has consistently shown us that this paradigm is very often not sufficient. If an expected ‘pattern’ doesn’t fit and ‘clear diagnostic markers’ are not found, the true source of unresolved symptoms must be somewhere else. This simple logic is what guides us toward solving a problem...LOOK SOMEWHERE ELSE.
If the numbers were less convincing, perhaps behavioural/neurogenic pain/psychosomatic factors might be considered for such widespread and poorly explained symptoms. Sure – pain behaviours and some psychosocial situations will contribute to patient-reported symptoms, but the widespread unresolved symptoms in and around the shoulder are reported by most chronic shoulder patients and they are consistent. Is it not logical to consider that another anatomical source may be contributing to these consistent and poorly recognized conditions?
Respected and experienced members of established and well-recognized professions within the medical community are experts in their fields. They are very skilled in identifying and managing patients who have conditions with clear diagnostic markers. The patients presenting with ‘shoulder’ conditions that do not present with a specific diagnosis are also recognized because many patients present this way. These ‘non-specific’ shoulder patients are recognized, but they do not have a diagnosis.
As a result of the ‘non’ diagnosis, the treatment plan becomes non-specific. Pain management, exercise, and lifestyle changes are suggested and because no specific ‘solution’ is offered by their medical practitioners, many patients will seek help where they can get it. Those without the financial or personal freedom to do so, will not follow up at all. Epidemiological studies confirm that among those struggling with a chronic shoulder problem, women outnumber men, and the largest cohort is consistently the older population.
Do we really understand “the shoulder”?
Like so many things…the answer depends on your point of view.
If we continue to use a single, simple term to identify an enormous, complex mechanism, expect there to be no change.
Problems in this region are always disguised.
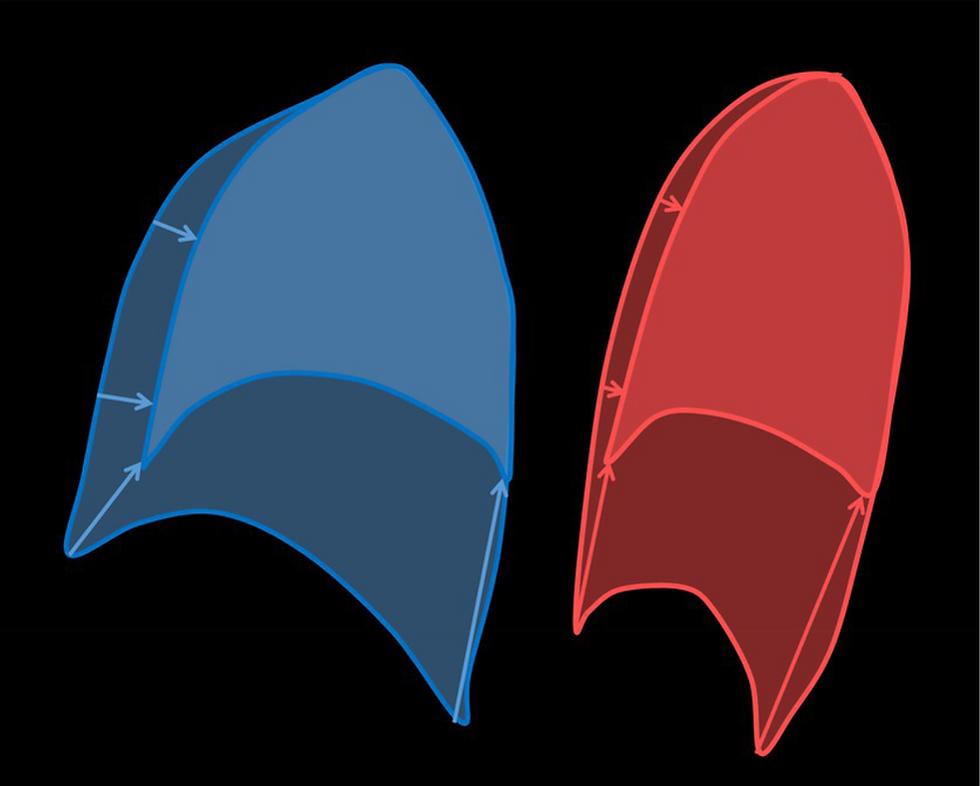
There is a complex and poorly understood mechanism that manages arm attachment with the body. This essential, dynamic, and fascinating link is the key that connects the arm with the body and yes – we experience problems with this mechanism all the time. We just cannot identify them. Problems in this region are always disguised. They can present as ‘non-specific pain’ or ‘fatigue’ or ‘shoulder pain’.
If we continue to look only at the glenohumeral joint, we will only find glenohumeral problems. Repair and rehabilitation of an injury to visible structures in and around the glenohumeral joint does work. Those who fit the surgical criteria generally have good outcomes. But – most people with ongoing shoulder problems do not fit the surgical criteria because their problem lies somewhere else. If serious pathology and problems with the cervical spine are ruled out, the likely source of many ‘shoulder’ problems will lie within this poorly understood arm attachment mechanism.
The “arm attachment mechanism” is the primary topic in my first book “Scapulothoracic Assessment in Three Simple Steps”. It requires an open mind and some imagination – as it should if we are to take a “new” look at a problem that currently goes unrecognized.
If you are suffering from an undiagnosed, non-specific shoulder problem and looking for answers… Stop looking. No one has the time or the resources to investigate something that is so poorly understood. When new information or new ideas do present themselves, there is virtually no chance of surviving the tidal wave of information that swamps the vast technical and research systems that exist today. A well-documented case history or case study – such as mine, cannot compete. This is unfortunate because the ‘case history/study’ has historically been an important source for new research. Now we rely on meta-analysis…
"My arm felt disconnected..."
On a personal note, my transition from a full-time, orthopaedic physiotherapist’ to ‘a patient with an undiagnosed ‘shoulder’ problem’ was the biggest learning experience of my life. Everything I thought I knew about the shoulder was wrong. My arm felt disconnected, and no one listened. Practitioners simply assessed my ‘shoulder’ (AKA – glenohumeral joint). It took years to grapple with and eventually gain some understanding about what exactly had happened deep within my shoulder girdle and the journey was not made easier by the fact that I was a physiotherapist. I was simply an older woman with a chronic shoulder injury.
Everyone is too busy staying in their lane...
Even now, after nearly 12 years of study, learning and writing, my attempts to share this unique and practice-changing knowledge have been unsuccessful. No one is interested. Everyone is too busy staying in their lane, too focused on their path to see the significance of what I have been trying to share.
...first-hand experience was necessary to recognize the gaps that exist in traditional anatomical/biomechanical teaching for this region.
One ongoing symptom that is the result of my injury (LTNP) is fatigue. As I have become older, fatigue is more and more difficult to deal with, despite ongoing exercise and a healthy lifestyle. I am now 65 years old, and I am too tired to continue with this research and writing effort.
I was hoping to help those like me – the patients without a diagnosis. I was sure that other practitioners would share my enthusiasm. My enthusiasm to share new knowledge. I finally had a clear understanding of scapulothoracic movement and control. Something that no other practitioner understands because first-hand experience was necessary to recognize the gaps that exist in traditional anatomical/biomechanical teaching for this region.
Book 2 – 'The Mysterious Winging Scapula', offers unusual advice, and it works.
Despite over 30 years in the business of helping people with these symptoms, I never really understood them, nor did I understand how to manage them until I lived with the problem.
I don’t have all the answers, but I HAVE MANY – if anyone cares to read what I have written. Book 2 – The Mysterious Winging Scapula offers unusual advice, and it works.
For those who do not have time to read what I have shared in my two books, I have a series of educational videos offered through Embodia: https://embodiaapp.com
Signing off
Janet Delorme






Comments