The Thoracic Connection
- Janet Delorme
- Mar 26, 2025
- 28 min read
Upper, middle and lower...An integrated masterpiece of biomechanics and motor control.
My last blog suggested that another path of exploration should be considered if a change to the current epidemiological statistics for chronic, non-specific shoulder pain is to be expected. "If clear diagnostic markers are not found, look somewhere else..."
Understanding the Functional and Interactive Thorax can provide insight that could potentially change our approach in assessing, treating and managing many conditions currently classified as neck or shoulder problems.
A comprehensive review of the thorax is not an easy topic, nor can it be summarized in a few short sentences. This is my longest blog, but it is cumulative and summative. While not yet fully elucidated, our understanding of the thorax is improving.
By Incorporating knowledge about multiple systems, we will start to recognize the 'integrated' thorax. This broad-based approach is required if our goal is to begin to understand the mysteries that lie within the masterful design of this region.
So, sit down, relax, and read. Be ready to look beyond the traditional mindset that plagues the thorax, and begin a journey toward further discovery.
Blog 12 - The Thoracic Connection
Part 1
The arm and its intimate connection with the thorax is the foundation for upper extremity function. While nerve roots originating in the cervical spine provide most of the motor and sensory nerve supply to the arm, the thorax is its true mechanical partner.
Hidden connections within the thorax provide the stability and power necessary for efficient coordination and transfer of movement and control throughout the human kinetic chain (KC).

M. Delorme - 60 m Portland Oregon, 1978
Coordination between the upper and lower extremities enhances transverse thoracic rotation, stride length, and, ultimately, walking or running velocity. The upper and lower extremities, working together, create optimal performance.
This 1978 photo shows us how a competitive sprinter utilizes his upper and lower limbs to achieve optimal speed. While the connection between the upper limb, the 'trunk,' the lumbar spine, the pelvis, and the lower extremity is evident, research is just beginning to provide some evidence that sheds light on the workings of the human KC.
A systemic review of electromyography studies by (E. Richardson et al. 2019) found that "...integrating the KC during shoulder rehabilitation may increase axioscapular muscle recruitment, lower trapezius muscle ratios and reduce the demands on the rotator cuff." Results consistently suggested that sequential lateral weight transference through the lower limb may be key to eliciting higher lower trapezius activation levels.
Serratus anterior (SA) was more difficult to study. The upper and middle fibres are too deep to access, so they are never used during EMG testing. The lower fibres are more exposed but difficult to isolate using surface electrodes. Rib movement accompanying arm elevation and thoracic spine range of motion creates additional challenges for consistent EMG readings.
Among the studies that did show SA participation, ALL showed significant activity with weight transference or unilateral loading through the lower limb. The authors stated that it could be argued that the differences in favour of KC exercises were underestimated. With the addition of stepping and the arm immobilized, the Smith et al. study measured the highest level of SA activity across all studies (199% MVC), when compared with bipedal stance.
These EMG findings are promising, but we are still far from understanding the diverse and complex relationship between the thorax and the upper limb.
'This review found evidence that integrating the KC (trunk and lower limb exercise) during shoulder rehabilitation may increase axioscapular scapular muscle recruitment'. (Richardson et al.)
Shoulder rehabilitation is nearly synonymous with shoulder exercise. Incorporating the KC into shoulder rehabilitation has long been recognized as beneficial for many recovering from shoulder injuries.
Unfortunately, many with chronic, non-specific shoulder conditions respond poorly to shoulder exercise programs. While the addition of KC rehabilitation may improve overall fitness, these patients continue to struggle with a 'shoulder' condition that remains troublesome and poorly understood.
As I said earlier...
"If clear diagnostic markers are not found, look somewhere else..."
Note: 'Core' and 'Kinetic chain' are popular and frequently used but lack consistent definitions. They are used here, as they often are, to convey a concept rather than a concise and clearly defined term.
The thorax is not the trunk
The 'trunk' is a term that is often substituted for the word 'thorax'. For example: 'Core stability is defined as the ability to control the position and motion of the trunk over the pelvis to allow optimum production, transfer and control of force and motion...'
Physiotherapists who utilize a neurophysiological approach to their therapy identify the pelvis and thorax together as the 'trunk' and the upper and lower limbs as the 'extremities.' Using functional techniques, postures, and motor learning principles, they facilitate proximal trunk stability for distal controlled mobility. 'Trunk' refers to a 'core' that has two primary focal points—the thorax superiorly and the pelvis inferiorly.

What is the thorax?
The term 'thorax' refers to the thoracic spine, the manubrium, the sternum and the xiphoid process, their associated 12 pairs of ribs and the non-contractile elements that provide the connections (joints, capsules, ligaments, articular and hyaline cartilage).
How does it move?
When studying human ergonomics for the United States Airforce in 1955, Dempster concluded that the human structure was an open chain system with several closed kinematic chains, such as the rib cage. (Butler 2003)
While we no longer think that the thorax represents a fixed, or closed chain, we do not fully embrace what IS known about thoracic movement.
When we picture the human thorax, many still visualize a fixed, articulated human skeleton, as seen at Halloween parties or in an anatomy lab.
For those who recognize the importance of thoracic mobility, evidence-based research that illustrates and quantifies thoracic motion remains limited.
The thorax provides mobility, but it also provides power and stability.
This multi-functional role must be considered; a two-pronged approach is needed.
We must understand that movement is:
Allowed, supported or restricted by the non-contractile elements (bones, ligaments, tendons, discs and cartilage). (osteoligamentous)
Initiated, stabilized and controlled by the contractile elements (neuromuscular).
(The neurological system might be considered a third element, because it coordinates and manages all systems.)
Osteoligamentous or non-contractile elements
Complex biomechanics of the non-contractile thorax have made research of this region difficult. However, some studies exist, and combining this evidence with clinical findings of internationally recognized researchers and clinicians Panjabi MM. 1976
D. Lee – Manual therapy for the thorax -1994, The thorax - an integrated approach 2003, 2014 and (LJ Lee 2013) does provide a framework.
D. Lee and LJ Lee state that thirteen articulations, their ligaments and connecting ribs form a typical 'thoracic ring.' For example, the fifth ring comprises the fifth and sixth ribs with their anterior attachments, T4 and T5 vertebrae and the T4/5 disc.
..."the intact thorax is mobile in all planes. The primary movement of the thorax is rotation, followed by lateral bending, with significantly less flexion and extension range of motion". (LJ Lee)
The living, functional thorax has many essential roles.
Its most familiar role, often assumed to be its only role, is protection for the cardiovascular and neurological structures that lie within it. This cage-like structure increases the stiffness of the thoracic spine and the critical buckling load by a factor of three or four. The costovertebral joints are credited as the most important stabilizers of the thorax (Oda et al. Spine 1996). However, normal function exposes the thorax to loads far exceeding those used to test thoracic stiffness in a lab.
As a result, additional forces from neuromuscular support are essential. (LJ Lee 2013)
The neuromuscular element
While the complexities of thoracic biomechanics have made research difficult, the compound,multi-sourced motor control in this region is labyrinthine by comparison.
As a result, research may never fully unravel the unique neuromuscular control that blends and coordinates multiple neurological systems... the central nervous system (CNS) with the peripheral nervous system (PNS), voluntary movement with autonomic movement.
Peripheral autonomous control of the viscera, smooth muscle (blood vessels), and sweat glands does not directly contribute to motor control. Still, the sympathetic and parasympathetic systems, largely contained within the thorax, can have an indirect effect and can be impacted by trauma or dysfunction within the thorax.
Motor Control is an area of research that has expanded exponentially since I studied neuroanatomy and neurophysiology. My updated understanding of this subject is limited to continuing education, clinical experience, and most recently, personal experience—my apologies for the gaps, inaccuracies and inconsistencies in this segment.
My unique neurological challenges, resulting from a poorly understood condition, have been the source of much inspiration. Careful observation, repetitive personal trials, and consistent documentation over many years have provided data that may not be of research quality, but I am the only person on record with LTNP who is capable of and willing to share personal findings with a professional perspective. My educated, experienced insight provides a rare and valuable contribution to improving the understanding and management of long-term complex conditions in and around the shoulder.
Introducing the DRIVERS*
*The term 'driver' is used here to describe a force created by movement /momentum, transferred to adjacent connecting tissues...like a slinky or a domino.
Human movement requires a complex mix of voluntary and autonomic control that can be instantaneously modified, adjusted or altered based on human needs, thoughts and the external environment. As a result, all movement combinations for each individual are impossible to anticipate.
We can recognize patterns and sequences of movement based on careful observational study. If one body part initiates movement and the movement appears to move in a specific direction, creating movement further along the 'chain' like a slinky or a domino, the source of the movement might be identified as the 'driver.'
There are multiple, complex drivers when considering the motor control of the thorax. Many are triggered autonomously, and most but not all of these autonomous triggers originate deep in the sub-cortical regions of the brain and the brainstem.
Autonomous triggers provide reflexive movement that we take for granted. They move our body in response to visual, auditory or vestibular stimuli and ensure that our body continues to 'autopilot' while we are otherwise occupied.
Recent research has identified two major groups of cortical neurons, located within six different layers of the cortex. Each layer has layer-specific processing. CStr (Corticostriatal projection) neurons are widely distributed across the cortex and can project ipsi or bilaterally. These motorneurons are associated with action selection, motor control, sequence learning, habit formation and more. Further research is needed to clarify the details and significance (Shepherd et al. 2014). An earlier study by Beloozerova et al. 2003, was done on animals. Their results indicated that the activity of many neurons within certain layers of the motor cortex is strongly correlated with changes in posture and gait.
Very interesting new developments. My previous understanding was that all motor projections from the cortex provided what we understand to be 'voluntary' control. Now, the evidence is showing us a much more complicated system.
While drivers have three possible levels of control (voluntary, autonomous or semi-autonomous), almost all neuromuscular control of the thorax is either autonomous or semi-autonomous. The thorax has limited voluntary control. Active movement of the head, neck or extremities (voluntary) facilitates or DRIVES the appropriate response within the thoracic spine and ribs (autonomous).
Muscles that support the thorax are mostly semi-autonomous. Nerves supplying the scapulothoracic muscles and the first intercostal muscle have no cutaneous branch. They work autonomously to provide postural and antigravity support to the upper thorax and scapula. However, they can also be controlled actively... when we 'shrug' the shoulders, up, forward or backward, for example.
(This concept is discussed further in Book One.)
Thoracic Driver #1
Respiration (the diaphragm) - primary thoracic driver (autonomous control>>voluntary)
Respiration is managed autonomously. The rate and pattern of breathing are regulated by nuclei in the pneumotaxic centre, located in the upper part of the pons (brain stem). We have semi-autonomous control because we can temporarily override this autonomous function (holding our breath, for example), but like the other life-sustaining organs that occupy our thorax, their control is ultimately autonomous. Their regulation relies on a balance of sympathetic and parasympathetic stimuli.
Breathing triggers anterior and posterior rotation of the ribs...
(Beyer B. et al. In vivo thorax 3D modelling... 2014).
Ribs 1-7 posteriorly rotate in full inhalation, and anteriorly rotate in full exhalation.
The mean helical axis for rib rotation ran anterolateral and inferior approx. 45 degrees to the mid-transverse plane.
Movement of the thorax (thoracic rings 1-7) can be initiated and stabilized by respiration.
Breathing provides the strongest mechanism for elevating the manubrium/sternum. The breath IN is synonymous with the contraction of the diaphragm. This triggers a spinal extensor response, which will extend the vertebrae and posteriorly rotate the adjacent ribs. The contracting and descending diaphragm creates a vacuum that allows the lungs to expand and fill with air. The result is increased stability of the thorax. Posterior rotation of the ribs that directly connect with and elevate the manubrium and sternum will contribute to the stability of the upper/mid thorax.
Notice when you try to open a tight pickle jar lid using 100% effort. You take a big breath, and you hold your breath while you perform your strongest upper extremity effort.
The problem with breath-holding with effort is obvious.
How can the active, upright upper thorax be stabilized without breath holding?... We will circle back to this. For now, recognize that the mechanical process of breathing is our first DRIVER for thoracic movement.
Part Two
Examining the Thorax by Region
To investigate multiple systems operating within the thorax, unique characteristics are best identified when we examine the thorax by region. Defining exact boundaries for these regions will depend on which characteristics are being examined. Functional boundaries are, however, quite simple: upper thorax, middle thorax and lower thorax.
UPPER THORAX - The gateway to the thorax T1, 2 (3)
The upper thorax provides the supporting framework for the mechanical, neurological and vascular systems that supply, move and stabilize the entire upper body. The neurological 'hub' in the upper thorax additionally provides safe passage for the autonomic and peripheral nerve supply to the distal regions of the body.
Thoracic Driver #2
Upper thoracic drivers: Head, Cervical Spine, Shoulder 'girdle' (autonomous > voluntary control)
Autonomic reflexes are triggered by sensory systems and proprioception. A loud noise, a sudden change in position, a change in visual direction, head position or neck position... All will trigger or 'drive' a response. Examples are spinal flexion, spinal extension, inspiration, expiration, or arm elevation. All triggered responses are movements that impact the position and, therefore, the stability of the thorax.
The head is a driver because it is THE command centre. Voluntary control dominates our extremities' everyday use, but the thorax (and the shoulder girdle) rely on a unique blend of cortical and subcortical control. Voluntary and autonomous movements that together provide for our safety, our survival and the management of our everyday needs.
The head is also a mechanical driver. Movement forward, backward or to the side will take the cervical spine with it, like a heavy ball at the end of a slinky.
The head can act as a mechanical driver, initiating cervical and then thoracic movement, but the head and neck play a much more significant role in managing the thorax because they are a primary source of autonomous control.
Cervical flexion and extension initiate primary flexor and extensor responses necessary for postural control. These movements trigger muscle support and balance for the entire upright spine.
When compared with the thoracic and lumbar spine, the cervical spine has, by far, the most mobility. This mobile conduit that links the head to the thorax is intrinsically unstable. Most of its strength and support are derived from its larger muscles - anchored securely onto the first and second thoracic ribs, the thoracic spinous processes, the sternum, the clavicle, and the scapula.
From a mechanical perspective, the zygapophyseal joints at the lower cervical and upper thoracic spinal segments transition in shape, allowing movement from the cervical spine to continue downward. Sidebend and ipsilateral rotation, for example, will start in the cervical spine and then continue down as far as the upper segments of the thoracic spine.
Unless countered by other forces, the weight of the head falling forward will continue to contribute to sequential flexion throughout the entire spine.
Extension, resulting from the head falling backward, will stop at the T1 junction due to the significant length of the C7 and T1 spinous processes and the abutting thoracic curve with shingled lamina. Sidebend and rotation suffer the same fate unless an additional force assists in changing the architecture at the CT junction as the spine extends.
When you sit up and assume an upright posture, control of the head, neck, upper thorax, and shoulder girdle is managed autonomously. The erector spinae, local spinal extensor muscles and the upper/middle fibres of key scapulothoracic muscles will lift the head, the neck and upper thorax. Visual and vestibular nuclei check and correct posture by communicating with receptors in the cervical and upper thoracic spine, and the upper/middle scapulothoracic muscles. This response contributes to an upright posture for the entire spine. However, there is a mechanical barrier at the top of the thorax where the T1 ring forms a 'yoke' that will remain angled downward - like a trap door that defaults to the flexed position.
WHY? ... Protection. Unimpeded spinal extension is dangerous, especially as the cervical spine approaches the thorax. Excessive extension, rotation, and sidebend will cut off the blood flow through the vertebral artery. However, a depressed manubrium/sternum will suppress active movement and mobility in the thorax and the upper extremities. Also, the subclavian artery, subclavian vein and brachial plexus travel between the clavicle and the first rib, and if this region is not elevated as the thorax and upper body start to work into upright, active postures, these neurovascular structures will be compromised.
We need a local safety/stability mechanism that will elevate the manubrium/sternum as we assume an upright/active position. Holding in a full breath of air can only offer very short-term assistance.
As discussed earlier, Breathing IN will automatically lift the manubrium and posteriorly rotate the first rib. However, an autonomous mechanism, in addition to respiration, must be in place to ensure continuous stability and support in this region
.
Most of our day is spent upright using the arms, often with force, usually well below shoulder height. Like the leading edge of a slinky, the anterior aspect of the T1 ring must lift before the remaining segments can follow. Lifting the manubrium to rotate that first ring posteriorly needs more than just spinal extension. It needs a lever.
A thick, sturdy muscle needs to span the first (and second) rib and attach to its (their) superior, anterior/lateral surface(s).

The thick, finger-shaped upper branch of serratus anterior (UBSA) provides the necessary lever.
It is composed of 7 fascicles from the superior surface of rib 1 and 8 fascicles from the superior surface of rib 2 (R2S) (Webb et al. 2016). This powerful, piston-like muscle can work from reverse origin and it can behave like a shunt muscle, creating significant compression between the superior/medial corner of the scapula and the anterior/lateral margins of the first two ribs.
I have explained McConnail's 'spurt and shunt muscle' theory in a paper (See - Other Publications on this site - Upper serratus anterior the hidden powerhouse - ODR 2017).
UBSA, acting like a LEVER, has shunt muscle capability. It produces compression and by doing this, it improves stability across the upper thorax and scapulothoracic articulation. The fibres of both rib 1 and rib 2s pass posterior and superior to attach to the anterior surface of the superior angle of the scapula (Webb et al. 2016). Much like the brachioradialis (a shunt muscle that stabilizes the elbow but also provides some uplift of the radius), the UBSA compresses and stabilizes the upper thorax while providing uplift of the manubrium.
The nerve supply of the UBSA is also unique (see Other Publications on this site - Upper Branches of the Long Thoracic Nerve - ODR 2017). The fascicles of the first and second rib are supplied by a separate branch of the long thoracic nerve. One that is supplied primarily by (C4),C5* nerve root. Several studies of the LTN confirm that the LTN has many variations in pathways, number of branches and contributing nerve roots. There is a consistent pattern, however, and with the lower branch, C6 and (C7) provide the primary nerve supply to the middle and lower parts of the SA.
Why the distinct difference at T1,T2? - The upper thorax and the UBSA play a distinct and unique role when considering the neuromuscular and biomechanical requirements at this juncture. Unlike the middle and lower parts of the thorax, this region MUST operate almost continuously during an active, upright day.
*C5 - a 'hybrid' motor nerve root?
C5 is the primary nerve supply for the upper branch of the SA. It also supplies the deltoid and the dorsal scapular nerve (levator scapula and rhomboids).
C5 'motor' control can be voluntary, but these 'voluntary' muscles also provide postural and reflexive action.
With our updated understanding of the multi-layered complexity of cortical control, this idea of a 'hybrid' motor nerve root may be something that needs further investigation.
At the T1 - T2 junction, the bony architecture, muscular morphology and nerve supply are distinct and unique when compared with the rest of the thorax.
This distinctive design provides essential support and motor control that is necessary for a fully functional thorax and upper extremity.
The autonomic control provided by the upper branch of LTN must be nearly continuous. The visible, lower parts of the serratus anterior are supplied by the lower branches of the LTN, where the input is triggered segmentally as the thorax extends and the arm starts to elevate.

The UFSA do not act alone in stabilizing and providing the necessary elevation to the upper thorax. Like all of our evolved and refined human mechanisms, there is considerable backup. Anti-gravity is handled primarily by a strong extensor response, but this will only support the spinal elements of our skeleton. Scapulothoracic/axioscapular muscles assist in supporting the upper thorax as well as the scapulothoracic region, but many will only operate on an 'as needed' basis.
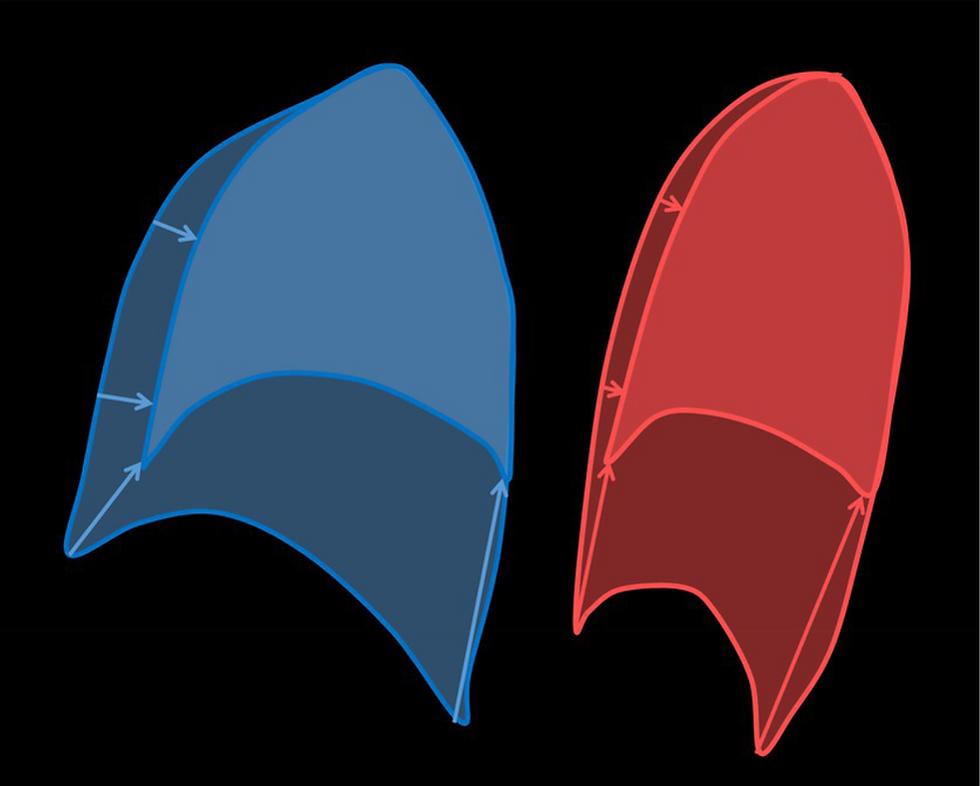
As shown in this diagram, the upper and middle trapezius work with UFSA to balance the forces around the upper thorax and the arm attachment mechanism. The scalenes, the rhomboids and levator scapulae (not shown) are also muscles that contribute to this effort.
Upright posture - AT REST - should require only minimal muscular effort.
Observe and palpate: upper trapezius, scalenes, sternocleidomastoids...sometimes they feel 'tight,' and sometimes they do not. These muscles are used intermittently during the day and only become continuously 'tight' if there is increased or sustained activity of the trunk/upper extremity, physical or psychological pathology, or muscle imbalance.
I have serratus anterior palsy (SAP) on the left. ( ...and NO - this is not a rare diagnosis - it is RARELY DIAGNOSED - more details in Book One and my next, hopefully final, blog).
Sitting up first thing in the morning, the right trapezius and scalenes feel soft and relaxed. The left trapezius and scalenes do not. The throat feels relaxed on the right but 'tight' and 'restricted' on the left. On a good day, the deep ache in the mid/medial scapular/rib region and axilla will not start until about mid-day. Symptoms will depend on my level of activity that day and the days previously, how long I am upright, and how well I have slept.
Video - stability within the upper thorax and shoulder girdle - with and without the contribution from serratus anterior.
Visual presentation of unstable and normal upper thorax/scapula during slight arm movement - left (SAP) compared with the right (Unaffected)
On the unaffected right side, the scapula maintains a stable relationship with the thorax as the arm swings through small arcs of movement. The left arm, performing the same small swinging movements, shows some scapular dyskinesis. There is not enough dyskinesis to be noticed during most standard shoulder examinations.
This small difference is generally overlooked because when assessing the 'shoulder' we are usually measuring 'shoulder ROM'. We are looking at the big movements - for example: What is the ROM - how far can you lift the arm overhead?
Mild scapular dyskinesis, as illustrated here, is often overlooked in most 'shoulder' assessments.
These small arcs of motion are typical, everyday movements of the arm - actions that are often overlooked due to their unassuming role in our daily activities... brushing your teeth, pushing your hair away from your face, adjusting your glasses, turning a page in a book or document, driving, fastening a seat belt, preparing a meal, hanging up your coat, or reaching for something on a shelf.
This mild, unassuming scapular dyskinesis accompanies almost every arm movement throughout the day. Combined with gravity, time, and frequency, this mild dyskinesis can result in inflammation and dysfunction that impacts both the shoulder and the cervical region.
The stability of the upper thorax and all daily, ubiquitous shoulder functions rely on the support established when an upright position is maintained. This is not an actively controlled 'shoulder' movement but an autonomic mechanism providing antigravity support and stabilization that is crucial throughout your upright day.
When the arm begins to elevate and move away from the thorax, a similar mechanical problem presents itself in the mid-thoracic region. The erector spinae can lift and support the spine, but additional power is needed to lift, support and posteriorly rotate the thorax as it accompanies mid-thoracic extension. To do this, a strong scapulothoracic connection is required to overcome the persistent flexion that dominates this kyphotic region of the thorax. Serratus anterior provides most of this strong connection. With the ribs now securely anchored to the upper extremity via the scapula, a new, powerful driver can contribute to the strength, range of motion and stability that is essential for a fully functional upper limb....the arm.
MIDDLE THORAX - The Crossroads - T(3), T4-T8 or 9
The central sections of the thorax exhibit the 'typical' structure of ribs and vertebrae.
Steeply sloping laminae are well suited to providing a large sweep of rotation while also allowing some side bending, flexion and extension. The apex, or mid-point of the thoracic kyphotic curve, lies at T6/7.
In this region, the middle and lower branches of the serratus anterior have individual groups of fascicles attaching to each rib from T3 (middle) to T8 or 9 (lower).
Several studies have investigated regional biomechanics of the thorax, and it is perhaps the regional biomechanics that will provide the most valuable data about the thorax because regional movement is FUNCTIONAL.
These two studies measured thoracic movement initiated with bilateral arm elevation. (Edmonston 2012, Tachihara and Hamada 2019)
Edmonston et al. utilized radiological investigation to measure total thoracic kyphosis (from T3-T11) during bilateral arm elevation.
The Tachihara and Hamada study measured the moving distance of ribs (mm) as arms moved overhead. Details are provided in Blog #7, where I introduce the concept that the scapula can move WITH or without the ribs...However, it is only when they move together that the thorax is stable and the power of the human kinetic chain is intact.
The video used in Blog #7 (link at the end of this section*) illustrates thoracic stability with and without the participation of the SA. It also shows rib movement accompanying arm elevation and trunk side flexion, with and without SA.
The R2 - inferior branch (R2I) of the SA is the largest fascicle, but it flattens and becomes very thin as it spreads to cover almost the entire anterior surface (fossa) of the scapula.
R2I passes horizontally to its rib attachment. The R2I and R3 fascicles combine to form the intermediate branch of SA. The role of this branch is to connect the ribs with the anterior aspect of the scapula (the fossa) and to provide a connection between the upper and lower parts of the SA (Webb et al. 2016).
Individual branches of the LTN supply the lower branches of SA. Working from reverse origin (like the upper fibres), their long, inferior/lateral trajectory ends with an attachment on the superior/lateral aspect of ribs 4-8 (or 9). Lower fibres of serratus anterior contract segmentally, and as the arm is elevated, the ribs lift (posterior rotation). Two possible mechanisms stabilize the elevated ribs:
The lower branches of the serratus anterior behave like shunt muscles, increasing compression and, therefore, stability through each rib as it is lifted.
The serratus anterior and the abdominal obliques, working from opposing sides of each rib, can stabilize them like opposing teams, pulling on a tug-of-war rope.

Serratus anterior, attaching to the superior/lateral border of ribs 4-8(or 9), works concentrically to assist in elevating the ribs, or eccentrically to control the lowering of the ribs when the abdominal obliques begin to contract with increasing force. Like a tug-of-war rope, each rib is supported and held in place by two well-matched, opposing forces.
Losing the top half of this well-designed force couple leaves a poorly supported thorax that can still expand normally with respiration at rest. The ability to perform and sustain ACTIVE expansion of the thorax will not be evident on a standard X-ray or with a thorax at rest. The primary driver - respiration - remains functional. The ability to elevate the ribs and stabilize them using ALL drivers (primary and all secondary) will be lost if the serratus anterior is ineffective or not participating fully. The functional thorax integrates multiple drivers, and the region where this integration is the most vital is the middle thorax - THE CROSSROADS.
*Video from Blog # 7
Thoracic Driver #3
Mid-Thoracic Driver: The upper extremity or THE ARM
(Autonomous and voluntary control)
The Drivers from above and below will assist the thorax primarily in the cervical and lumbar transitional zones. Within the mid-thorax, the largest zone, another driver is required to support and manage the movement patterns for which this region was designed.
Rotation (Rtn) and sidebend (SB), coupled with flexion and extension. The spontaneous coupling of Rtn/ SB with flex/ext provides our thorax with the versatility needed to coordinate multiple drivers, enabling a fluid and seamless interaction with our environment. Our ability to use our arm, supported by our thorax, allows maximal reach, push, pull, twist, and turn. A strong, adaptable and fully functional upper limb requires instantaneous support from a constantly changing blend of thoracic movement.
When ' locked in' with the thorax via a stable connection with the scapula, the ARMS can drive the thoracic range of movement, enabling our full human potential. Our arms cannot achieve full functional ability when acting alone, and the thorax, without reinforcement from the upper extremity, loses power and range of movement. One enhances the other.
This is not a new concept. Proprioceptive Facilitation was a therapeutic approach to motor learning that was first developed by Dr. Herman Kabat in the early 1940's. Physiotherapist Dorothy Voss added the word 'Proprioceptive' to give us the name we are familiar with today. In 1945, Maggie Knott joined Kabat and Voss, and Knott began teaching Physical Therapists (Physiotherapists) the unique patterns and techniques of PNF. The first book was authored in the early 1960's (Knott and Voss), and to this day, physiotherapists continue to use the classic diagonal upper limb and lower limb functional patterns of movement, where facilitation from the extremities feeds into central nerve impulses that can excite, inhibit or strengthen muscles on a neurologial basis. History of PNF. International PNF Association https://www.ipnfa.org/organisation/history-of-pnf
The extremities are 'drivers'. Their contributions are evident every day.
We can now measure intervertebral thoracic SB and Rtn using In vivo 3D computed tomography (Fujimori T. et al. 2012) (Fujimori T. et al. 2014). However, these studies are done in supine, where the functional role of the thorax is not represented. Sitting up off the flat testing surface will add gravitational force to the thorax, triggering primary, autonomic drivers. Lifting the arms and bringing in the upper extremities brings in additional forces from upper extremity drivers.
The mid-thoracic region, at the apex of the thoracic kyphosis, is the region that is most vulnerable to reduced mobility due to changes in the spine. Changes that can be attributed to age, sexual orientation or illness. Loss of mobility in this region will result in compensatory efforts by its drivers: #3, Upper limb...usually resulting in a 'shoulder injury, and #2, Head, Neck and Shoulder girdle...usually resulting in 'neck and upper back' pain or headaches. Interesting correlation with epidemiological data for unexplained, chronic neck and shoulder conditions...
Grasping the concept of the functional thorax requires an understanding that goes beyond anatomy and biomechanics. The mid-thoracic 'Crossroads' represents the true centre, where all drivers have representation. Motor control, with its complex source of 'drivers,' lies at the centre or the 'heart' of this complex system. The importance of this central 'Crossroads' or 'Heart' is not limited to knowledge acquired from the teachings of Western Medicine. Traditional Chinese Medicine (TCM) has, for over 3,000 years, recognized that a vital substance resides within the 'Heart' or 'Shen' region. 'Shen' - is considered a vital substance that plays a crucial role in emotional and mental well-being. This is an interesting parallel with the sympathetic and parasympathetic systems, which provide essential elements intrinsically linked to our vital 'core'.
Demonstration - Thoracic Rotation - modified by using arm position and/or arm movement. Try this yourself...
In upright sitting, feet resting flat on the floor and arms resting at your sides, rotate as far as you can to the right, and then to the left, allowing the head and neck to drive the rotation as far as possible. Pick a visual marker to establish the end of your range of movement.
Now, elevate your arms to 60-70 degrees abduction, then repeat the rotations. Do not pull with the arms, just hold them in place like you would if you are balancing. You will notice a significant increase in movement. Then go ahead and allow the arms to assist with the rotation.
The arm participates as a driver without actively pulling. The abducted position alone has engaged the scapula with the thorax. Adding active arm participation further enhances this powerful mechanism.
LOWER THORAX - The Power Converter - T 8-10 (false) and 11, 12. (floating)
The ribs beyond T8 or T9 no longer have serratus anterior attachments. These ribs do not attach directly to the sternum. T8-10 ribs attach to T7 costal cartilage, and the much shorter T11 and 12 ribs have no anterior connection with the thorax. This transitional architecture, forming a wider, more open and flexible inferior thoracic margin, suggests an increased ability to absorb torque and rotational forces.
Thoracic Driver #4
Lower thoracic driver: Lumbar spine/lower extremity
(autonomous and voluntary control)
Much like the transition between the cervical and thoracic vertebrae, the zygapophyseal joints at the lower thoracic and upper lumbar segments also transition for optimum transfer of motion. The lumbar spine has less flexion and extension ROM than the cervical spine but much more flexion and extension than the thoracic vertebrae.
The lumbar spine allows very little rotation, so while rotation and flexion/extension from below can be guided and fine-tuned at the zygapophyseal joints, the primary driving force from the lower extremities must be converted from a movement that is, for the most part, in the sagittal plane to a rotational force that is primarily in the transverse plane. This conversion from a sagittal to a transverse force is performed by the muscles connecting these two regions. The oblique abdominals and the serratus posterior inferior connect the lower lumbar vertebrae to the lower thoracic ribs and act like a 'bridge,' allowing large rotational forces to transfer between the thorax and the lumbar spine. (This is consistent with EMG findings where 'stepping' resulted in the highest levels of activation of SA and lower trapezius. (E. Richardson et al. 2019.)
The thorax can be influenced by motion from below, as shown in this gait analysis drawing.
Observe the diagram below: The right lower limb is in late stance, and the right hemipelvis is in a position of right rotation in the transverse plane. The degree of pelvic rotation will increase as stride length increases.
The thorax and upper extremity, in response, will counterrotate left, smoothing out the centre of gravity and assisting in maintaining a head-forward position.

The goal of human locomotion is to move the body forward in space while the movement of individual segments is such to maintain minimal displacement of the centre of gravity (CG) in the vertical and lateral directions. (Tucker et al. 1998)
While normal gait relies on the 'drive' provided by the powerful muscles of the lower extremity (Driver #4), the dynamic stability and control required for a smooth and coordinated gait require multiple sensory inputs, including somatosensory, visual and vestibular inputs, as well as spinal reflexes and cortically controlled movement patterns (Tucker et al 1998). (Driver #2)
Does Driver #3 - the upper limb, play a role in normal walking and running?
At slower walking speeds (0.8 m/s* and lower), there is a shorter stride length and minimal or no arm swing. The upper and lower extremities advance in the sagittal plane, more or less in phase with each other, and at a frequency ratio of 2:1 between the arm and the leg. At walking speeds higher than 0.8 m/s, stride length and arm swing increase, and the arm swing moves out of phase, gradually synchronizing with stride frequency. (Ford et al. 2007)
*0.8 m/sec = 2.88 km/h
This observation suggests that increased speed will increase stride length, creating increased forces from below that will 'trigger' the out-of-phase trunk/pelvis rotation.
The Pelvis - The equalizer or neuromuscular way-station

The lower half of our neuromuscular 'core.
Capable of three-dimensional movement and has 36 muscle attachments.
Its 'basin' protects, supports and manages the normal function of the lower organs.
It is the focal point for parasympathetic supply in this region (mirroring the Vagus nerve, which is the parasympathetic source in the head and upper organs).
Balances and coordinates forces
between the lower limbs and the thorax.
Multiple forces in three dimensions will act simultaneously during gait, so a simplified example is used here to help explain the interaction of the muscular forces above and below the pelvis:
Powerful right hip and knee flexion drives the right hemipelvis into posterior rotation (sagittal plane). This will trigger an opposing force in the pelvis, meant to slow, control and balance this change in pelvic position. Erector spinae will contract, as will the abdominal obliques (left external and right internal). Myofascial connections in the thorax, between the external oblique and serratus anterior will trigger the lower branches of the serratus anterior to contract. The upper branch is already in play because our person is upright, and Driver #2 is assumed. The arm is not elevated, but it has been "locked in" with the thorax by a trigger that comes from the lower extremity driver - Driver #4.
The more powerful the forces from below, the more active the responding drivers need to be. Slow walking requires very little compensatory activity and, therefore, very little compensatory thoracic rotation. Very fast walking requires active compensation, and sprinting needs the power from the upper limbs to respond by contributing to the counter-rotation. Much like the video example provided in the previous segment - Thoracic Driver #3 - Mid-Thoracic rotation), the power from the arms can contribute to trunk rotation, and they do this when the forces from the lower limbs are very high, and the power required for counterrotation, necessary for attenuating these forces, must also be very high if they are to maintain a smooth centre of gravity and an efficient transfer of energy for forward propulsion.
Until we start to recognize the magnificent biomechanical and neuromuscular interactions within the thorax and between the thorax and the rest of our body, we may never be able to move beyond models like the one below....

I have no personal video here to demonstrate my limited left-arm swing.
Subtle changes in trunk rotation are difficult to see and even more difficult to spot when the body is in motion. - perhaps a job for a researcher looking for a clinical study...
When walking at a brisk pace, I do notice the very limited left arm swing -the trapezius is still doing what it can to draw the left shoulder girdle posteriorly as the right leg swings forward, but the arm never swings beyond the midline of the sagittal plane. The trapezius can initiate the posterior swing, but it is not able to 'hand off' the job to the serratus anterior at the mid-line. They are meant to work together. (details in Book One - Scapulothoracic Assessment in Three Simple Steps - pp 22-24).
I also notice that the top of the left shoulder (the acromion) lifts at mid-stance and drops back down at mid-swing. Rotation within the left thorax is not effective for attenuating the vertical displacement from below. The arm feels like it has since 2012...disconnected from the thorax.
Summary...
The drivers from above have the biggest influence on spinal flexion/extension and autonomic control, but it is the driver from the middle that can significantly influence stability, movement and power throughout the functional kinetic chain. A stable and mobile thorax, integrated with the upper extremity, can support the cervical spine and engage with the lumbar spine, pelvis and lower limbs to create optimal performance.

The upper and lower extremities, working together, create optimal performance.
Final Remarks
I hope that this review of the 'Thoracic Connection' has provided some perspective about how the integrated thorax impacts not only our everyday activities but our everyday LIFE.
The most overwhelming losses that many people experience are the ones that are currently not recognized. The initial 'injury' is not recognized for what it truly is. No one listens because no one understands, and, for the most part, the message many patients receive is: "You 'look fine,' so get on with your life." The problem is you do not know how to do that.
Since 2012, I have struggled to maintain a positive spin on life. While motivation is scarce at times, I continue to exercise (a very modified routine - see my Book 2), and I adhere to principles I have learned by reading several books that teach me how to live better and longer. In the book I am currently reading, 'Outlive' by Peter Attia, the author uses an example of an older, active, fit and happy woman who fell and injured her 'shoulder.' Unable to recover from this, she was unable to enjoy any of her usual activities. She went on to develop neck pain, back pain, depression, dementia, respiratory infection, and then death - 15 years after the initial shoulder injury. The author speaks of not only increasing lifespan, but improving our healthspan.
This example spoke to me because this is EXACTLY the person I am writing for and about.
Some have pain; some do not. Some will have shoulder complaints, but some may present with a variety of complaints that seem to be unrelated.
Diane Lee, a physiotherapist who has specialized in thoracic biomechanics for most of her career states...
Understanding the biomechanics of the thorax is critical for understanding its role in multiple conditions since the thorax is part of many integrated systems including the musculoskeletal, respiratory, cardiac, digestive and urogynecological...understanding the biomechanics is fundamental to all forms of treatment for multiple conditions. D. Lee 2015
Recognizing that other systems (neural, myofascial, visceral) may be contributing to ongoing difficulties with the treatment and management of the thorax, D. Lee and colleagues utilize an Integrated Systems Framework (ISF) model, where a patient-centred approach focuses on finding the primary source of the problem.
This insight, suggesting a new approach to the management of the thorax, is very promising, and, for the first time since suffering a long thoracic nerve injury 12 years ago, I have a reason for some optimism moving forward.
While long thoracic nerve injury cannot explain ALL problems with the thorax and the chronic shoulder, it can explain SOME. Building on a better understanding of the complex and diverse role of the serratus anterior and the long thoracic nerve, we can continue to improve our understanding of the thorax and its interactions with the human kinetic chain.
Better recognition will lead to better management for those whose healthspan, and likely their lifespan, has been impacted because of their unrecognized, undiagnosed condition.




Comments