The Shoulder - Unclassified
- Janet Delorme
- Sep 3, 2023
- 5 min read
Blog 9
Epidemiology of the Shoulder - Part 2
Today, we will complete our discussion on shoulder diagnosis and classification, and we will briefly review the last two topics on this Epidemiology Cycle Chart, below:

Moving on to a new paradigm? – We will get there in Blog #10.
The Shoulder UNCLASSIFIED
Evidence-based shoulder classification systems, generated between 1990 and the early 2000s operated on two key assertions:
1. Clinical testing, performed by a wide range of medical professionals with an equally wide
range of training, education, and clinical experience, will never provide consistent and
reliable results, especially if seeking a specific pathoanatomic diagnosis.
2. A simple clinical examination is sufficient to initiate appropriate treatment and
management.
Walker-Bone, 2002., recognizing these difficulties when diagnosing soft tissue disorders of the neck and upper limb stated …
The importance of making a diagnosis lies in its utility in distinguishing groups of patients who require different case management, and diagnoses that carry different prognoses or different associations with modifiable risk factors.
K Walker-Bone et al. 2002
A specific shoulder diagnosis may not be identified. A good history, appropriate screening for ‘Red flags’ (more serious pathology that may present with shoulder pain), and a simple,
reproducible physical examination combined with attention to modifiable risk factors should provide enough information to move forward with patient management.
In 1999, with a growing trend for moving away from a medical model for diagnosis, Physiotherapists were encouraged to assess and treat their patients based on a disablement model. The American Physical Therapy Association went so far as to state this in their 1999 Guide to Physical Therapist Practice. (Alexandria, Va: APTA; revised July 1999.):
The Guide is based on a framework that rejects the medical model of disease (which emphasizes 'treating the diagnosis') and that focuses instead on the process of disablement.
The rationale for rejecting the medical model for disease in favour of a disablement model is: When applied to a wide range of patients, whose condition is chronic or complex, a medical or pathoanatomic model will often underperform, leaving many with insufficient or ineffective treatment options. A disability model, taking a more broad, psychosocial approach, will often assist in the management of those who demonstrate nonorganic signs, overt pain behaviors, elevated fear of physical activities, or excessive pain somatization. This either/or rationale was controversial, with some medical professionals voicing strong opposition.
R. DiFabio, former Editor-in-Chief of JOSPT, responded to this growing trend with a powerful statement piece: “Disablement: The Patient’s Problem No Longer Matters”
DiFabio spoke for many professionals who believe that biomechanics and anatomy provide an essential, structural basis for the diagnosis of movement-based disorders...
” Pathoanatomical models of disease have lost our favor recently and have been replaced
with a framework for providing care that de-emphasizes diagnosis… Models of disablement
have removed the pressure to search for offending structures, leaving us with the mindset that the cause of the patient’s symptoms does not matter.”
Responding to comments from Mark Werneke, DiFabio did agree that the best approach for patient treatment and management is one that combines both models, much like Waddell’s Biopsychosocial model of disablement for low back pain.
Research during the early 2000s has improved our understanding of pain, shoulder imaging and special tests. We now recognize that shoulder diagnosis cannot be classified simply as organic (Pathoanatomic) AND/OR non-organic (Disablement Model).
Ludewig et al. 2022 report that those with advanced pathologies such as full-thickness tears or arthritis, continue to rely on a pathoanatomical diagnosis, but for many patients with shoulder conditions, the movement away from a pathoanatomic diagnosis remains the trend because:
1. There is often a lack of connection between tissue pathology and pain.
2. Pain processing can be very different from one individual to the next.
3. Often there are multiple tissue pathologies around the shoulder.
4. Diagnostic imaging is costly and of uncertain value.
5. Limited value of clinical “special tests”.
6. Influence of a ‘label’ on patient expected outcomes and perceived need for treatments
such as surgery.
As a result, pathoanatomic diagnosis for many shoulder patients remains unattainable. Ludewig et al. 2022
Effectiveness of Treatments
Despite the lack of clear diagnostic classification, medical professionals continue to identify their shoulder patients using some variation of the original Codman/Cyriax system. Screening, Assessment tests and diagnostic procedures have been updated and modified, but the basic principles have not changed. For example: review the two recent assessment algorithms presented in Blog #2.
As a result, the treatment and management of shoulder conditions are largely based on the original four pathoanatomic classifications.
There is evidence to support the efficacy of conservative management (exercise, manual
therapy) for some shoulder conditions (Hawk et al. 2017., Pieters et al. 2009)
However, “…most outcomes do not demonstrate fully resolved symptoms or positive outcomes for all individuals.” Ludewig PM, Borstad JD. 2003, Ludewig et al. 2022
Outcomes and Prevention
If the theoretical epidemiological “cycle” (as shown at the top of this Blog) is working as it should, comparing data from the earliest epidemiological shoulder studies with data from equivalent, more recent papers, should indicate a trend or a change.
Two recent epidemiological studies (Hodgetts et al. 2021, Lucas et al. 2022)
Report that:
- Shoulder pain continues to be prevalent in older populations that are still working,
particularly if their work is physically active or involves the use of their upper limbs.
- Prevalence rates ranged from 10.8-55.2% for a period of 12 months or more.
- A ‘significant proportion of the population across the world will experience shoulder
pain daily, yearly, and throughout a lifetime.’
Both epidemiological studies reported methodological limitations. These limitations are attributed to classification and widely differing methodological and statistical
approaches. Epidemiologists can improve their methodological and statistical approaches to the study of shoulder conditions, but they cannot change how shoulder conditions are diagnosed or classified.
Prevalence data from recent epidemiological shoulder studies, despite improvements in research scope and methodology, remains essentially unchanged when compared with earlier studies.
Unclassified shoulder problems continue to disable a significant proportion of the population, and risk factors, both modifiable and unmodifiable, are consistent. For example, higher prevalence for women, older adults and those who perform repetitive upper limb/overhead work/sport.
Epidemiological data can provide a general picture of this globally disabling condition, but it cannot provide diagnostic or classification-based data. Until we find an accurate, inclusive and consistent method of identifying this region of the body, we will continue to wrestle with something we do not fully understand.
This epidemiological cycle is stalled, because Diagnosis/Classification remains the weak link, hampering progress through the last two stages: Effectiveness of Treatment and Outcome and Prevention.
A system of clear guidelines for the classification and diagnosis of shoulder
conditions has been and will continue to be unachievable until we are able to
recognize and understand a new paradigm.. a new pathoanatomic model.
Perhaps we are approaching this from the wrong point of view…
Are patients not appropriate for the classification system? Or…
Is the classification system not recognizing the pathoanatomic diagnosis hidden within the patient?
The models presented and utilized in practice have not YET provided us with a workable classification system, but …”the design of human anatomy often conceals pathology”(DiFabio, 2000).
We cannot ignore the relationship between anatomical structure and function. Ongoing research, exploring biomechanics, anatomy, morphology and clinical science, encourages and challenges us to think again about a pathoanatomic model. A new model.
We are making inroads toward a more inclusive pathoanatomic shoulder model.
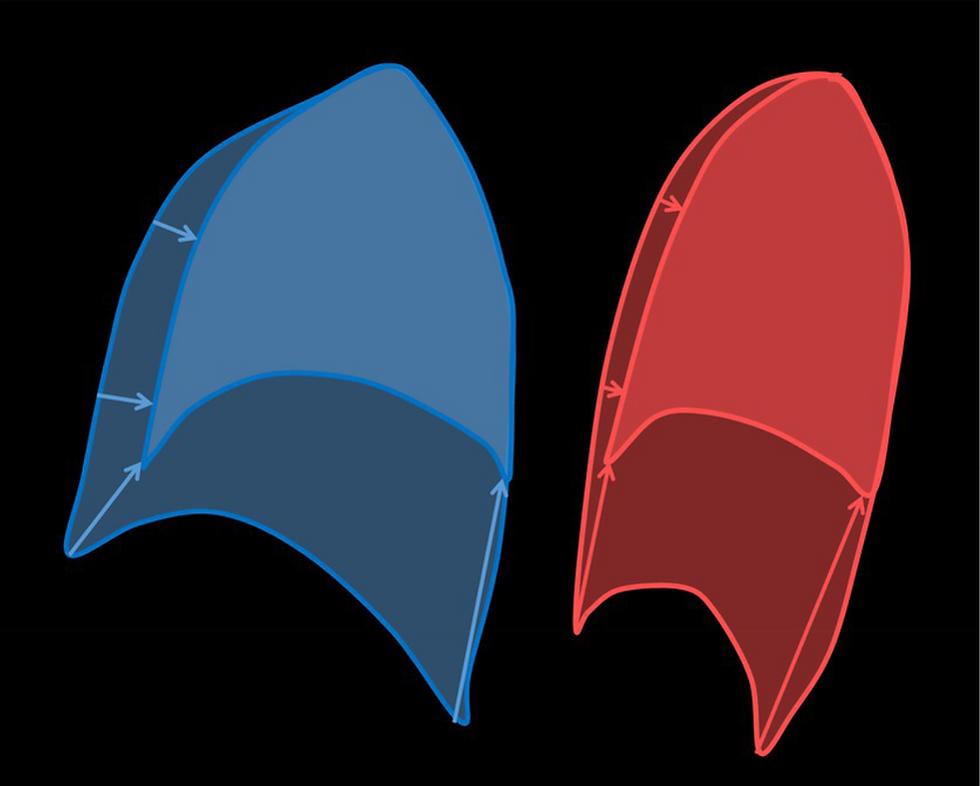
For example, multiple research papers, many by Ludewig et al., contribute significant new information about scapular movement and position relative to humeral movement and position. Some of this new information is presented by Ludewig et al. 2022 in this shoulder pain classification flowchart:

This classification system is the beginning – the first classification system to identify primary
scapular movement dysfunction as a contributing cause of shoulder pain.
Observing scapular position and movement relative to humeral position, however, has not and will never be a clinical tool that can provide enough reliable evidence for a diagnosis (Blog #5). It is, however, an excellent starting place. Using a different paradigm, research and clinical testing could provide momentum in the progression of our ability to recognize, assess and manage the entire shoulder joint complex.
Blog #10 The Shoulder – A New Paradigm? will present the big picture. I hope you are ready for it… and yes, I will incorporate and explain the purple text throughout these last two posts!
Coming soon...



Comments