Epidemiology and the Shoulder
- Janet Delorme
- Aug 25, 2023
- 9 min read
Updated: Aug 26, 2023
Part One...From the Beginning
Epi- upon
Demos - people
Logos – study
Epidemiology …the study of what is upon the people.
Modern epidemiology is said to have started when Dr. John Snow traced the 1854 cholera outbreak in London to a single water pump. Since this time, epidemiology has become the medical specialty that tracks disease or conditions by prevalence (how many cases at a specific time), and by incidence (how many cases over time). Epidemiological research tracks the distribution and cause of diseases or disorders within groups of people and contributes knowledge on how to prevent or manage diseases or disorders. Their data answers the basic questions: Who is sick? What are their symptoms? When did they get sick? and Where could they have been exposed? Epidemiological studies of people with shoulder pain were scarce prior to the 1980s, but today (August 2023), A Pub Med search using the keywords Shoulder + Epidemiology will cite 8,236 papers.
Before the 1980s, shoulder complaints were often simply considered to be ‘shoulder complaints’, and while they did impact people’s lives, the accepted belief (fractures and dislocations aside) was that shoulder pain either got better or it did not. With varying degrees of success, people simply learned to live with shoulder pain, dysfunction, or disability. Family doctors were only seen when necessary and their advice for shoulder pain was often … ‘rest, wait and see’. Shoulder surgery, and treatment provided by other health professionals such as physiotherapy, were available in larger centres, but most people, especially those from smaller communities or rural areas, continued to rely solely on their family doctor for the management of their shoulder problems.
Medical specialties have expanded over the past fifty years to include rheumatology, neurology, orthopaedic surgery, physiatry and occupational health. Health professional practices such as physiotherapy, occupational therapy and chiropractic therapy have also become more widely available, offering many treatment options for patients with shoulder conditions. Patients with shoulder pain are now seeking treatment and their expectations for recovery have changed.
Shoulder pain and disability have likely always been a source of significant morbidity* but it has only been since the 1980s that epidemiologists have started to investigate this condition.
*Morbidity is another term for illness. A person can have several co-morbidities simultaneously. So, morbidities can range from Alzheimer's disease to cancer to traumatic brain injury. Morbidities are NOT deaths. Prevalence is a measure often used to determine the level of morbidity in a population. (New York State Department of Health.gov)
The earliest epidemiological studies investigated shoulder pain as it relates to disability, age, manual labour, occupational workload, and economic and psychological factors. (Cunningham/Kelsey, Herbets et al.1984. Chard/Hazleman1987, Bergenudd et al.1988.)
Shoulder pain, especially among those of middle age or older, was having a significant impact on our ability to work. It soon became clear that shoulder conditions were very prevalent and their impact on ‘the people’ was significant. It was also in the late 1980s when epidemiological publications about sports-related shoulder conditions started to appear. (Jobe et al.1989.)
From 1990 to the present day, epidemiological studies about the shoulder have grown exponentially and new research, exploring the “who, what, when where and why” of shoulder pain and shoulder disability has flooded journals (medical, orthopaedic, pain, spine, physiotherapy, rehabilitation, ergonomic, occupational and environmental health, rheumatology, sport and epidemiological) from around the globe.
Why so much data? What is driving this epidemic of epidemiological study?
Epidemiologists collect and use data to estimate or learn more about the…
frequency
causes
diagnosis
effectiveness of treatments
outcome and prevention… of shoulder conditions. (Buchbinder et al.1996)

If this systems cycle operates as it should, epidemiological data can assist healthcare professionals in making their decisions about the management of a specific problem.
Good data provides answers that should lead to change.
Better management = better outcomes
…HAS there been a notable change in the who, what, when, where or why of shoulder conditions over these past fifty years?
We should start from the beginning…
Epidemiologists began their research by determining prevalence…How many people struggle with a shoulder condition?
Using population-based research, and self-administered questionnaires epidemiologists asked participants for specific information. The results from one of the largest early studies
(T. Hasvold./R Johnsen 1993) estimated the prevalence of shoulder/neck pain to be 15.4% for men and 24.9% for women. It was concluded that disabling headache, neck and shoulder pain are highly prevalent, and many do not seek professional help.
Subsequent population-based studies have demonstrated consistent prevalence numbers. Linaker et al.2015 report that “…shoulder pain affects 18-26%. …of adults at any point in time, making it one of the “most common regional pain syndromes.”
During the 1990s and early 2000s, several large, non-specific prevalence studies were published in the UK and the Netherlands. While there was some variation in incidence rates, the overall numbers presented a consistent message:
- Shoulder complaints are the third most common musculoskeletal complaint in primary care. (Winters et al. 1999, Urwin et al. 1998.)
- The prognosis for shoulder complaints is unfavourable. Chronicity and reoccurrence are common (Winters et al. 1999)
- 50% recovery after 6 months, increasing to 60% after one year. (Kuijpers et al. 2004 Vanderwint et al.1996 Croft et al. 1996)
- 13% were still consulting with shoulder symptoms at the three-year follow-up. (Linsell et al.2015)
Shoulder problems are prevalent and, despite not always being reported to a primary health care professional, shoulder conditions are the source of significant pain and disability.
Prevalence data provides clinicians with information that helps them identify individual risk factors that may be important for the classification, diagnosis, and management of their patients. Age and sex, for example, have the most consistent and profound impact on prevalence, severity, and chronicity. Modifiable risk factors might include obesity, smoking, psychological factors, and repetitive, strenuous, or overhead work.
Classification and Diagnosis
“Diagnostic classification is the foundational underpinning of providing care of the highest quality and value.”
A system of clear guidelines for the classification and diagnosis of shoulder
conditions has been unachievable…
Bjelle 1989 and Buchbinder et al. 1996 provide many reasons for this interminable problem:
Shoulder complaints…
- often present with head, neck, arm or hand symptoms.
- result from a wide variety of conditions or diseases.
- can be identified or labelled in many different ways, using variable criteria for diagnosis.
Even if a specific condition is identified, the terminology is often different and many of the
terms have multiple meanings. (Bjelle 1989, Buchbinder et al.1996.)
A synopsis
Classification systems for the shoulder have gone through many changes since Amory Codman first introduced the four classifications of shoulder diagnosis in his 1934 book – “The Shoulder.” He presented a pathoanatomic (anatomy-based) classification that identifies rotator cuff disease, biceps tendon disease, adhesive capsulitis (frozen shoulder syndrome) and acromioclavicular joint abnormalities as the four primary diagnoses for shoulder pathology.
The most significant change to this classification system was presented by Dr. James Cyriax (1904-1985), a British-trained orthopaedic surgeon. His widely popular book, Textbook of Orthopaedic Medicine, Vol 1 – Diagnosis of Soft Tissue Lesions, has eight editions and was first published as Rheumatism and Soft Tissue Injuries. c1947, before being published under its current title in 1954.
Cyriax introduced ‘selective tissue testing’, a systematic examination that should identify a specific anatomical site—the biceps tendon for example.
Codman’s classification system, combined with Cyriax’s selective tissue testing techniques became, for many years, the most recognized system for shoulder classification and diagnosis.
Codman+Cyriax...A Summary: (Linaker et al. 2015)
Rotator Cuff Tendinopathy
- Degenerative changes by the fifth decade of life, particularly in the hypovascular “cuff” region.
- Degenerative changes – micro tears – macro tears = frequent cause of painful shoulder symptoms.
- May include Inflammation of tendons or bursa
- Pain worse when lifting arm – “impingement”
- Isolating involved tendon using selective tissue testing (James Cyriax) – however, evidence is lacking.
Biceps tendinopathy
- Prone to tendinopathy
- Most use Cyriax criteria: anterior shoulder pain, local tenderness over tendon, pain on resisted elevation of the arm and/or isometric flexion of the elbow.
- It is thought that biceps tendinopathy generally co-exists with rotator cuff pathology and impingement
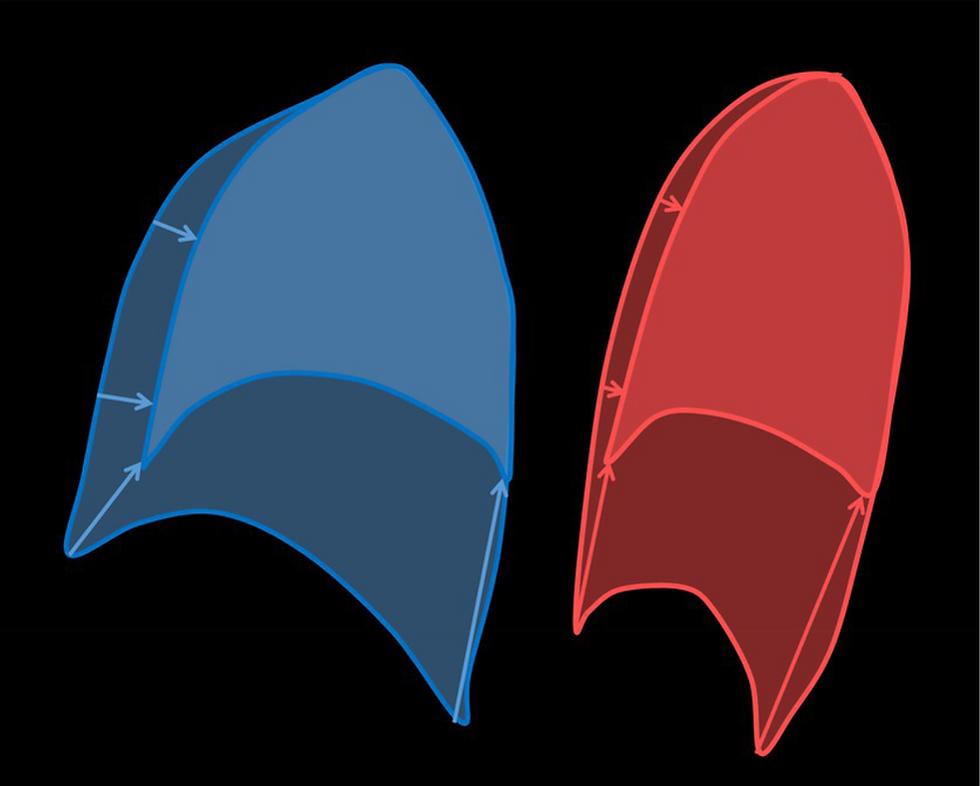
Adhesive capsulitis (frozen shoulder syndrome)
- “frozen shoulder” first coined by A. Codman, for a “class of cases which are difficult to define, difficult to treat and difficult to explain from the point of view of pathology”(Codman EA. The shoulder: Boston; 1934 [Google Scholar]
- Codman suggested primary cause was supraspinatus tendonitis, with inflammation then progressing to include remaining parts of the shoulder, including the joint capsule.
- This view is disputed and there is no agreement as to the true underlying cause of the “frozen shoulder”.
- Usually goes through three phases – acute - very painful, lasting 3-6 months, adhesive - pain resolves but movement of shoulder becomes more restricted, and resolution - range of movement and function at the shoulder are gradually restored.
- Average time - 30 months, but may be considerably longer, and it is not clear that complete recovery occurs, one study reports that 50% of patients did not recover full movement after 7 years.
- Diagnosis of ‘capsulitis’ – studies use inconsistent information, for example: limited passive ROM, External rotation reduced by at least 50%, passive ROM and active ROM, pain and limited ROM, duration. None of the studies included a definition of “normal” range of movement.
Acromioclavicular joint syndrome
- Diagnostic tests for this condition are well described, but in practice, studies of shoulder disorders have rarely included diagnostic tests specific to this condition.
This classification system has been taught, published, modified and widely used for at least fifty years. Clinicians’ findings, using this classification system, were found to be consistently unreliable, and as a result, there was much disagreement and confusion:
compared the clinical diagnoses of three rheumatology consultants, who all examined the same group of shoulder patients. Agreement between the three consultants about the specific diagnosis was achieved in less than half of the patients. They attributed this disagreement to two factors.
1. Patients presenting with more than one shoulder lesion made the diagnosis more difficult to ascertain.
2. Consultants had differences in interpretation of certain physical signs.
also studied interobserver agreement on the classification of shoulder disorders. Eligible patients with shoulder pain were recruited in various healthcare settings in the Netherlands. Patients were classified into one of six diagnostic categories: Capsular syndrome (including arthritis), acute bursitis, acromioclavicular syndrome, subacromial syndrome (tendonitis, chronic bursitis), rest group (unclear clinical picture, extrinsic causes) and mixed clinical picture.
Of the 201 patients evaluated, only moderate agreement was found on the classification of shoulder disorders. Patients with high pain severity, chronic complaints and bilateral involvement were the most difficult to classify.
These complex guidelines were not working. Patients presenting with severe, chronic or non-specific symptoms were often misdiagnosed or un-diagnosed.
This sub-group of patients is identified as having ‘non-specific shoulder pain’, which is described as ‘shoulder pain, discomfort, fatigue, limited movement and loss of muscle power but without a pattern allowing a specific diagnosis to be made’
Non-specific shoulder pain, frequently found in general population and workplace studies, is estimated to be six times more frequent than specific shoulder conditions with clear diagnostic markers - rotator cuff for example.
Linaker et al 2015, Boocock et al. 2009, Miranda et al. 2005
A more reliable classification system was required. During the 1990s and into the twenty-first century, researchers and multi-disciplinary experts combined their expertise to redefine shoulder disorders and diagnostic criteria. Extensive literature searches and improved epidemiological methods resulted in new examination tools. As a result, many new evidence-based classification systems were generated.
The NHG (Dutch) Practice Guideline 1990, (updated May 1999)
recognized that “a physical examination is not sufficient for determining which anatomical structure is affected”. Rather than identify a specific anatomical structure, the initial shoulder evaluation was simplified to include:
- A detailed patient history (anamnesis)
- A limited physical exam (inspection, neck range of motion, shoulder movements – active abduction, passive abduction, and passive external rotation)
Patients are initially identified as having a shoulder disorder and the problem is managed step by step, as needed: Advice, analgesics, local cortisone injection, then physiotherapy if there is a loss of function or the problem persists beyond six weeks.
Studies by Palmer et al. 1998, and Walker Bone et al. 2002 and
2004 also utilized a simplified shoulder assessment, with the goal of establishing a practical shoulder exam with a measurable standard of validity and repeatability (The Birmingham diagnostic criteria for upper limb disorders 1997). There were three diagnostic choices: Rotator cuff tendonitis, Bicipital tendonitis and shoulder capsulitis (frozen shoulder). However, there was often overlap - 205/410 subjects with adhesive capsulitis were also diagnosed with rotator cuff tendinitis and 23/28 people diagnosed with bicipital tendonitis also fulfilled the criteria for the diagnosis of adhesive capsulitis.
Other, more structured approaches to the classification of soft tissue disorders of the upper limb and neck were proposed, (Buchbinder et al. 1996) but they were also found to have problems. Some of the proposed systems were considered too elaborate, requiring special skills to perform the assessment, and some failed to demonstrate that the examination was adequate and accurate. These systems also failed to cater to patients who partially fulfilled the criteria or who had patterns of complaint that fell outside of the specified categories.
TO BE CONTINUED...
Epidemiology and the shoulder is a subject that cannot be fully addressed in one blog. The story continues with Epidemiology and the Shoulder - Part Two.
The shoulder - UNCLASSIFIED... are we ready for a new paradigm?
To be posted very soon.
**Keep track of the dialogue that appears in purple. A summary, presented in part two, will pull this information forward and use it to illustrate a consistent pattern over time.
Thanks for reading –
Janet Delorme



Comments