Why are we looking at the scapula?
- May 2, 2023
- 8 min read

Scapula (n.)
in anatomy, "shoulder blade," 1570s, Modern Latin, from Late Latin scapula "the shoulder," from Latin scapulae (plural) "shoulders, shoulder blades," perhaps originally "spades, shovels," on the notion of similar shape (or of the animal shoulder blades used as scraping tools in primitive times), from PIE *skap-, variant of *skep- "to cut, scrape"
From: Online etymology dictionary
On their own, the scapulae are shovel-shaped bones whose only prehistoric post-mortem purpose appears to have been that of scraping or shovelling. When integrated with the back of the chest wall in the living specimen, this unusually shaped, flat, and slightly curved bone becomes an essential part of a mechanism that is responsible for linking the arm to the body.
My last blog provided some historical perspective on the observational assessment of the shoulder, with a special focus on the scapulothoracic region. Since Inman et. al. introduced the scapular ‘setting phase’ and the 2:1 ratio of humeral to scapular movement back in 1944, the bulk of most subsequent ‘shoulder’ research has been centred around pathology, treatment, exercises, and surgical management of conditions that are primarily related to the glenohumeral joint. This is not to say that there has not been any progress made in the areas of research, clinical assessment, and management for the remainder of the shoulder girdle, because there has been some excellent work done in this area of study. Thanks to a dedicated group of clinicians and researchers, we are now much closer to understanding how altered scapular position and movement, or scapular dyskinesis, impacts the function of the upper extremity (this includes the glenohumeral joint).
No one denies the fact that the scapula has an important role in the normal function of the arm. Stability, strength, and movement at the ‘shoulder’ relies on the support, strength and movement that is provided within the shoulder girdle, especially at the scapulothoracic joint.
….”The scapula has a number of crucial roles, but most importantly, it serves as the link that transfers energy from the large muscles of the trunk, lower extremities, and core to the smaller muscles of the arm during arm movements”. (Sciascia 2012, 2022)
We recognize that the scapula has an important role. What we do not yet have an answer for are two important questions:
1. How does the scapula perform this important job?
2. How can we measure or identify whether the scapula is performing as it should?
Since 1944, we have continued to observe and measure scapular and clavicular movement.
Despite years of research and study, the exact link between dyskinesis and diagnosis remains a mystery. We know something important is going on, but we are not yet able to pinpoint how ‘it’ can be measured and validated.
There has been some progress of note in this area of research. This pair of studies, A Clinical Method for Identifying Scapular Dyskinesis Part 1: Reliability (McClure et al. 2009), and A Clinical Method for Identifying Scapular Dyskinesis Part 2: Validity (Tate et al. 2009) evaluates abnormal scapular position or movement patterns (dyskinesis) among a select group of young athletes. Test subjects for these studies were university-age (average 20.7 yrs.), primarily male (111/142 and 50/66), and most were competitive in overhead sports (water polo 89, swimming 19, baseball/softball 28, tennis and others 6).
Part one (McClure et al.) set out to determine interrater reliability for a test that was designed to detect abnormal scapular motion. Scapular dyskinesis was defined as the presence of winging or dysrhythmia. Scapulae were rated as normal, subtle, or obvious dyskinesis.
The test results suggested agreement between examiners (interrater reliability) in identifying dyskinesis 75-82% of the time.
In part two, using a similar, select group of overhead athletes, Tate et al. set out two objectives. First, they would determine the validity of the scapular dyskinesis test used in Part one, and second, explore the relationship between scapular dyskinesis and shoulder symptoms.
Several previous research studies, using electromagnetic digitization(3,35,36*), and electromagnetic sensors (4,9,28,37*), identify a specific pattern of normal scapular and clavicular movement as the arm is elevated. This ‘normal’ pattern of movement has the following kinematic descriptors: scapular upward rotation, posterior tilting, and external rotation, as well as clavicular retraction and elevation. Results from the Tate et al. study were consistent with the results from the previous studies listed above. (*References are listed in Tate et al. study)
The test subjects identified as ‘normal’ were compared with those identified with obvious dyskinesis. Those with subtle dyskinesis were not included.
This study, comparing kinematic differences between those who were identified as normal with those identified as having scapular dyskinesis, was deemed valid because it demonstrated differences in kinematics between those with and without dyskinesis. Participants with obvious dyskinesis showed less scapular upward rotation, less clavicular elevation, and greater clavicular protraction than those who were identified as ‘normal’.
The presence of dyskinesis, however, was not found to be related to shoulder symptoms. It should be noted that some participants did acknowledge SOME shoulder pain, but NONE felt that the pain was significant enough to require treatment or limit participation in their sport.
To summarize, we now have the technology to consistently measure scapular and clavicular position and movement, and these findings correlate reasonably well with clinical assessment, for those with obvious winging or dyskinesis…in a population of 20-year-old overhead competitive athletes, most of whom are male.
All studies have shortcomings, and it is customary to list them at the conclusion of each study. Like almost all studies I have read, these two papers suggest that “further studies” are recommended. The authors agree that we still need to establish a relationship between scapular dyskinesis and a diagnosis (symptoms/pathology), and we need to recognize that test subjects in these studies represent a unique demographic. Young, healthy, athletic males present with unique physiological characteristics, especially in the shoulder region. This is something we can expand on in a subsequent blog.
As a result of these shortcomings, the data from these two 2009 studies will likely not characterize most patients presenting with shoulder pain at primary care facilities.
Any suggestions for further studies?
I think we need to go back to the two questions listed at the start of this blog.
How does the scapula perform this important job?
The scapula performs this job because it can “link” the upper extremity with the core and ultimately with the lower extremities. Describing or even understanding how this “link” works may provide us with important insight. Looking for and measuring obvious dyskinesis has not, so far, provided the answers we need.
Maybe we should take a second look at the setting phase…
Inman et al. described the “setting phase” as the highly irregular, yet subtle scapular movement that occurs during the first part of arm elevation. Their rationale was correct, in that the muscles in and around the scapula are getting ready, and ‘setting up’ the scapula so it can do the job it is meant to do…transfer forces.
I struggled to find a ‘mechanical’ entity that closely mimics the role of the scapula. There is no perfect replacement for the scapula in the non-living world, but, like many living parts of the body, engineers have come up with some excellent ‘replacement parts’. In the case of the scapula, the best comparison I have found, so far, is with that of a coupler.
The basic function of all couplings is to transmit power, accommodate misalignment and compensate for axial movement (end movement of shafts). Sometimes, a coupling is asked to absorb shock or vibration.
Definition from: Altra Industrial Motion
With this definition, we establish an important concept. The scapula ITSELF is not the important part of the puzzle, the scapula behaving like a coupler, is one of two pieces (the clavicle being the second), that connect two very important structures. The UPPER LIMB and the AXIAL SKELETON, and more specifically, the ribs #1-8 or 9, depending on your individual anatomy.
We need to shift our focus away from the scapula itself, and instead, think about how this ‘coupler” works. We need to look at specific muscles, and even more important, we need to understand how the ribs need to behave if they are to provide the support and movement necessary for their complex yet essential role.
I used to imagine that the scapula was somehow “suctioned” onto the chest wall and that it was this intimate chest wall/scapula relationship that created this essential physical and functional “link”. I also used to imagine that the chest wall was a fixed destination - a secure landing place for the arm attachment muscles. Exactly how this link is created and stabilized was a mystery until I lost the link connecting my left arm.
Losing this ‘connecting link’ between the arm and the chest wall is a bizarre and disabling problem that is too complex and non-specific for the average person to describe.
Besides, our bodies are excellent compensators. We change how we use the arm; we adjust our activities, and carry on the best way we know how. That is ultimately what I had to do, but it took several years, and I had to give up my career and most of my active lifestyle.
Did I have scapular dyskinesis? Yes. Was it obvious? No.
The scapula “appeared” a little different, but nothing that would be considered unusual.
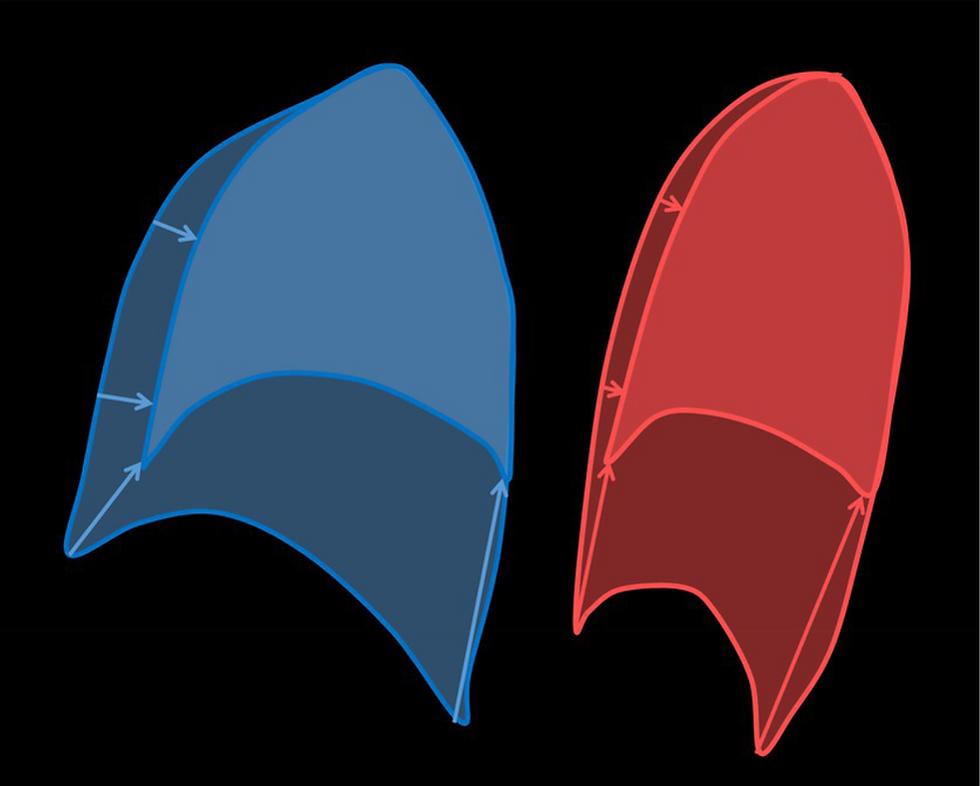
‘Disconnect' - observed ‘Disconnect’- imagined from the inside.
from the outside.


This “normal” scapular appearance was paired with:
A sense that the scapula had ‘disconnected’ from the chest wall and had shifted up and forward.
The distinct feeling of disconnect while actively walking. Right arm, swinging at the side of the body, perfectly counterrotating the movement generated in the legs and pelvis. Perfectly connected. Left arm, bouncing up and down while resting slightly forward of the midpoint of the hip (trochanter). NOT swinging normally. Disconnected.
A Physiotherapist cannot turn this stuff off. Ten years later and I still recognize this odd sensation. I have learned to live with it, but I cannot ignore it.
This ‘coupler’ was no longer grasping my chest wall, and I would later discover that one muscle was primarily responsible for the integrity of this essential link. Six important scapulothoracic muscles exist, but the serratus anterior has the most extensive, intimate connection.

This photo is from a 2005 study by Bertelli/Ghizzoni, where cadavers were fresh – not embalmed. Labels identify the three parts of the serratus anterior (U – upper, I – Intermediate and L-Lower). Lt identifies the long thoracic nerve. Notice the two distinct branches at the top of the photo, and multiple separate branches (Sb) supplying the lower fibres.
Serratus anterior, with its three distinct parts, provides the scapula with three dimensions of connection with the ribs. From its attachment along the full length of the inside (medial) border of the scapula, the thickest sections at the top and at the bottom corner, travel forward and down, toward the ribs (anterior/inferior). The thinnest, middle section, travels in a similar direction toward the ribs, but it passes directly in front of the scapula cloaking its ventral (front) surface. This very intimate connection of scapula/muscle can be seen in this excellent dissection photo, where the impression of the entire scapula remains clearly imprinted on the middle fibres of the serratus anterior after the scapula has been lifted off it.
A more recent morphological study of this muscle provides even more insight, but that is information for my next blog, where we investigate how forces are transferred to and from the upper extremity via our biological coupler – the scapula. Even more interesting will be a discussion that may help answer our second question: How can we measure or identify whether the scapula is performing as it should?
Stay tuned…Blog 6 is coming soon.


Comments